Pressure sores are excruciating and debilitating, and they can even lead to death. Elderly pressure sores are most common in people who are bedridden or have limited mobility. Usually caused by prolonged pressure on the skin, they affect over 2.5 million older adults each year. They are the leading cause of preventable hospital-acquired complications.
While caring for my elderly father, who was a stroke victim, I understood the importance of proper skin care. Although partially mobile, he spent long hours in his lift chair. We continued to keep him free of pressure sores with careful adjustments. Unfortunately, not all elderly help with this type of care. Some people don’t realize the importance of proper skin care.
Pressure sores can be a painful and dangerous condition, especially for the elderly who are bedridden or wheelchair-bound. Pressure sores, also known as bedsores or pressure ulcers, occur due to constant pressure on one part of the body.
In this blog, we will discuss everything related to pressure sores in the elderly, starting from what they are and what causes them. We will also cover identifying risk factors and recognizing early symptoms of pressure sores.
Furthermore, we will dive deeper into the various stages of pressure sores and how to treat them effectively. Prevention strategies such as regular movement, proper nutrition, and hydration will also be discussed.
Lastly, we will address some of the challenges caregivers face when dealing with pressure sores in their elderly family members and how they can best support them during this difficult time.
Contents
Understanding Pressure Sores

Pressure sores, called bed sores, are open wounds that form on the skin due to prolonged pressure. These sores occur when blood flow to a specific skin area is restricted, leading to tissue damage and pressure ulcers.
Older adults are particularly vulnerable to bedsores due to limited mobility, bony areas, and friction. Preventing pressure injuries in elderly patients involves proper skincare, cushions, and special mattresses. Healthcare professionals play a crucial role in educating patients and caregivers about preventing pressure sores.
Definition and Causes of Pressure Sores
Pressure sores, also known as decubitus ulcers, are skin injuries that result from sustained pressure on bony areas of the body. These bedsores are a common concern for elderly individuals with limited mobility, older age, and health conditions that affect the blood supply. Prolonged pressure can damage the skin’s underlying tissue and even reach the muscle and bone, leading to open wounds and dead tissue. Factors such as moisture, friction, shear, and friction contribute to the severity of pressure sores in older people. Additionally, bowel incontinence, urine, malnutrition, and dementia increase the risk of bedsores in elderly patients.
Identifying Risk Factors for Elderly Pressure Sores
Older adults with limited mobility, dementia, or incontinence face a higher risk of developing pressure sores. Age, disease control, malnutrition, friction, moisture, and sustained pressure contribute to bed sore risk in elderly patients. Healthcare professionals, including GPs, should assess patients for risk factors and provide appropriate guidance on pressure ulcer prevention. Regular skin inspections, mobility aids, healthy tissue, and moisture control can help reduce the risk of bedsores in older adults. Education of carers, patients, and healthcare professionals is crucial in mitigating pressure ulcer risk in elderly patients.
Credits: Rehealthify
Recognizing Symptoms of Bed Sores in Elderly Patients and Loved Ones
Recognizing symptoms of pressure sores in elderly patients is crucial for early intervention and preventing complications. These symptoms include redness, discomfort, tenderness, and changes in skin color. If left untreated, pressure sores can progress to open wounds, crater-like ulcers, pus, and damage extending through multiple tissue layers. Older adults may also experience complications such as cellulitis, septic shock, and limited healing. Healthcare professionals should regularly assess the skin, especially in areas prone to pressure sores like the buttocks, shoulder blades, and tailbone. Prompt intervention, proper dressing, antibiotics, and wound care are essential for preventing complications and promoting healing.

Early Signs of Pressure Sores
Early signs of pressure sores in elderly patients may include redness, skin discoloration, and warmth in specific areas of the body. It’s important not to ignore discomfort, tenderness, and mild skin damage in bony areas such as the buttocks, shoulder blades, and tailbone. Regular skin inspections, along with moisture control and friction reduction, can help identify pressure sores at an early stage. Carers, nursing staff, and healthcare professionals should remain vigilant in monitoring the skin health of elderly patients. Prompt treatment of these early symptoms can prevent complications, open wound formation, and further tissue damage.
Progression of Symptoms
If left untreated, pressure sores in older adults can progress from mild skin damage to open ulcers, pus, and dead tissue. As the severity of pressure sores increases, they extend through the epidermis and dermis and reach deeper tissue layers, affecting tendons, muscles, and bone. This progression of symptoms can lead to complications such as cellulitis, septic shock, and a long-term healing process. To prevent the progression of pressure sores in elderly patients, the healthcare team should implement regular skin inspections, risk assessments, and appropriate care, including carers, nursing staff, and healthcare professionals.
Stages of Pressure Sores

Pressure sores in elderly patients are categorized into different stages based on the severity of tissue damage.
- Stage 1 – Pressure sores involve mild skin damage, redness, and discomfort.
- Stage 2 – Open ulcers with pus and dead tissue are present, extending through the epidermis and dermis.
- Stage 3 – Pressure sores penetrate deeper tissue layers, affecting tendons and muscles, forming crater-like ulcers.
- Stage 4 – Pressure sores reach the bone, causing severe damage and posing higher risks of complications.
Monitoring and timely intervention are crucial to prevent progression and improve outcomes in older adults.
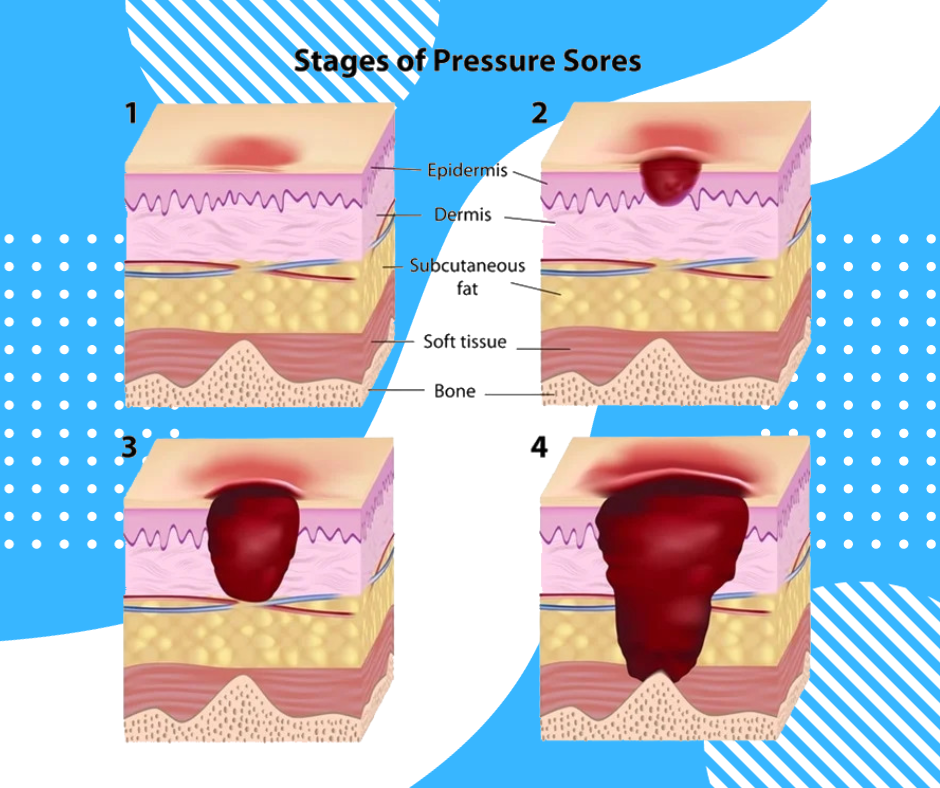
Stage 1 and Stage 2
Stage 1 pressure sores in older adults involve mild skin damage, including redness, tenderness, and discomfort, indicating tissue damage. However, there are no open ulcers at this stage.
On the other hand, stage 2 pressure sores are characterized by open ulcers, pus, dead tissue, and additional skin damage. These pressure sores extend through the epidermis and dermis of elderly patients. Effective treatment for stage 1 and stage 2 pressure sores includes prompt intervention, wound care, antibiotics, and moisture control.
Regular skin inspections, friction reduction, cushions, and the use of special mattresses can also help prevent the progression of pressure sores in older adults.
Stage 3 and Stage 4
Stage 3 pressure sores in older adults involve deeper tissue damage, affecting tendons, muscles, and forming crater-like ulcers. These ulcers are more severe than stage 2 and require prompt intervention.
On the other hand, stage 4 pressure sores are the most severe, reaching the bone and causing extensive damage. This stage poses a higher risk of complications for elderly patients. Treatment for stage 3 and stage 4 pressure sores includes debridement, antibiotics, dressing, wound care, and special mattresses.
Collaboration between healthcare professionals, carers, nursing staff, and patients is crucial in managing complications and promoting healing in older adults.
Treating Pressure Sores in the Elderly

Prompt and proper treatment of pressure sores in older adults is crucial to prevent complications, open wound formation, and further tissue damage. Treatment methods for pressure sores in the elderly may include debridement, antibiotics, wound care, cushions, special mattresses, and friction reduction.
Regular skin inspections, moisture control, and the use of mobility aids can help in the healing process. Healthcare professionals, carers, and nursing staff must collaborate in tailoring treatment plans for pressure sores in older adults. Additionally, educating patients, carers, and healthcare professionals about pressure sore prevention, treatment, and wound care is essential for effective elderly care.
Initial Treatment Methods
To ensure effective initial treatment for elderly pressure sores, it is vital to clean and dress the affected areas promptly to prevent infection. Applying appropriate wound care products, such as mild soap and specialized gauze or gel, can help promote healing. Additionally, using unique cushions or mattresses can relieve pressure on the affected areas and reduce further damage. Keeping the pressure sores dry and clean and regularly changing bandages and dressings to facilitate healing is crucial.
By implementing these initial treatment methods, elderly individuals with pressure sores can experience improved outcomes and a reduced risk of complications.
When to Seek Professional Medical Help
If pressure sores in the elderly show signs of infection or worsen despite treatment, it is crucial to consult healthcare professionals for assistance. They can guide advanced wound care options and help manage severe pressure sores. Immediate medical attention should be sought if pressure sores exhibit redness, pus, or open wounds.
Elderly individuals with spinal cord injuries or nerve damage may require specialized care. For health information and expert advice, reach out to healthcare providers with experience treating pressure sores.
Prevention Strategies for Pressure Sores
Encouraging older adults to change positions frequently can help relieve pressure and prevent pressure sores. Providing cushions or foam mattresses is another effective strategy to distribute pressure evenly and reduce the risk of developing sores.

Ensuring that older adults maintain good nutrition and hydration prevents skin damage and promotes overall health. Educating both older adults and caregivers about proper skin care routines is crucial. Regular skin inspections should also be promoted to identify areas of concern before pressure sores develop.
Importance of Regular Movement and Position Change
Regular movement and position change are crucial in preventing elderly pressure sores. Encouraging elderly patients to shift their body weight every two hours helps alleviate constant pressure on specific areas.
Mobility exercises improve blood flow, reducing the risk of bedsores. Special cushions are effective in reducing pressure on bony areas. Educating bedridden patients about the importance of repositioning in bed promotes better circulation.
Additionally, emphasizing the role of shoulder blades in redistributing weight can help prevent pressure sores. Incorporating these practices can significantly reduce the risk of developing pressure sores.
Role of Nutrition and Hydration in Pressure Sore Prevention
Ensuring older adults consume a balanced diet supports skin health while promoting hydration, helps maintain skin moisture, and prevents damage. Adequate protein intake is vital for tissue healing. We know that vitamins and minerals play a significant role in skin health. Caregivers need to encourage older adults to eat properly. Also, consult healthcare professionals for personalized dietary recommendations.
We can effectively prevent pressure sores and promote overall skin well-being by prioritizing nutrition and hydration. Remember to customize the diet according to individual needs and seek professional guidance for optimal results.
Challenges in Caregiving: Handling Pressure Sores
To effectively handle pressure sores, caregivers need to be educated on the risk factors associated with their development. They should also be trained in proper wound care techniques, including dressing changes, to ensure optimal healing.

Managing limited mobility in older adults is crucial in preventing bedsores. So, caregivers should be provided with guidance on repositioning and movement. Additionally, supporting caregivers in implementing pressure sore prevention strategies and equipping them with knowledge about special mattresses or cushions that reduce pressure can significantly contribute to better outcomes.
By addressing these challenges, caregivers provide the best possible care for individuals at risk of pressure sores.
How Can Family Members Best Support Their Bedridden Elderly?
Supporting bedridden elderly relatives involves regularly assisting with repositioning, promoting healthy eating and hydration for skin health, and collaborating with healthcare professionals for care plans. Also, providing emotional support and advocating for regular medical assessments of pressure sore severity and healing progress helps ensure the best results.
Preventing Elderly Pressure Sores
Preventing and treating pressure sores in the elderly requires a comprehensive approach. Caregivers need to understand the causes, risk factors, and early signs of pressure sores. Prompt treatment and seeking professional medical help when necessary are essential.

However, prevention is always better than cure. Regular movement, position change, proper nutrition, and hydration play a vital role in preventing pressure sores. Caregivers should also provide emotional support and create a comfortable environment for their bedridden elderly loved ones. By taking these steps, we can ensure the well-being and comfort of our elderly population and promote healthy aging.
Frequently Asked Questions
How can caregivers and family members help prevent and treat pressure sores in their elderly loved ones?
Encourage frequent position changes and avoid prolonged sitting or lying in one position. Regularly check the skin for signs of pressure sores, like redness. Keep the skin clean and dry, and use cushions to reduce pressure on bony areas. Consult a healthcare professional for advice and treatment options.
What are some signs of pressure sores, and when should I seek medical attention?
Signs of pressure sores include redness, swelling, tenderness, and open sores. Seek medical attention if the sore is pus-filled, has a foul odor, or if you experience fever, chills, or increased pain. Early detection and treatment are crucial to prevent further complications.
What are some treatment options for pressure sores in elderly individuals?
Treatment options for pressure sores in elderly individuals include wound cleaning and dressing. In severe cases, surgery may be necessary to remove damaged tissue or address underlying issues. Pain management can be achieved through topical creams or oral medication. Preventative measures like repositioning and padding can also help prevent further development of pressure sores.
What causes pressure sores in elderly individuals?
Pressure sores, also known as bedsores, develop in elderly individuals due to prolonged pressure on the skin and underlying tissue. Factors such as thinning skin, reduced mobility, malnutrition, dehydration, and incontinence contribute to their formation. Preventive measures like regular repositioning, proper nutrition, and maintaining clean and dry skin can help avoid pressure sores.
Learn More About Senior Parent Care!
Explore the world of senior parent care with us! Join our community on Facebook, Instagram, and Twitter for valuable insights, tips, and a supportive network dedicated to enhancing the lives of our senior loved ones.
Facebook: https://www.facebook.com/SRParentsCare
Instagram: http://instagram.com/SRParentsCare
Twitter: https://twitter.com/SRParentsCare
Together, let’s enrich the lives of our senior parents!