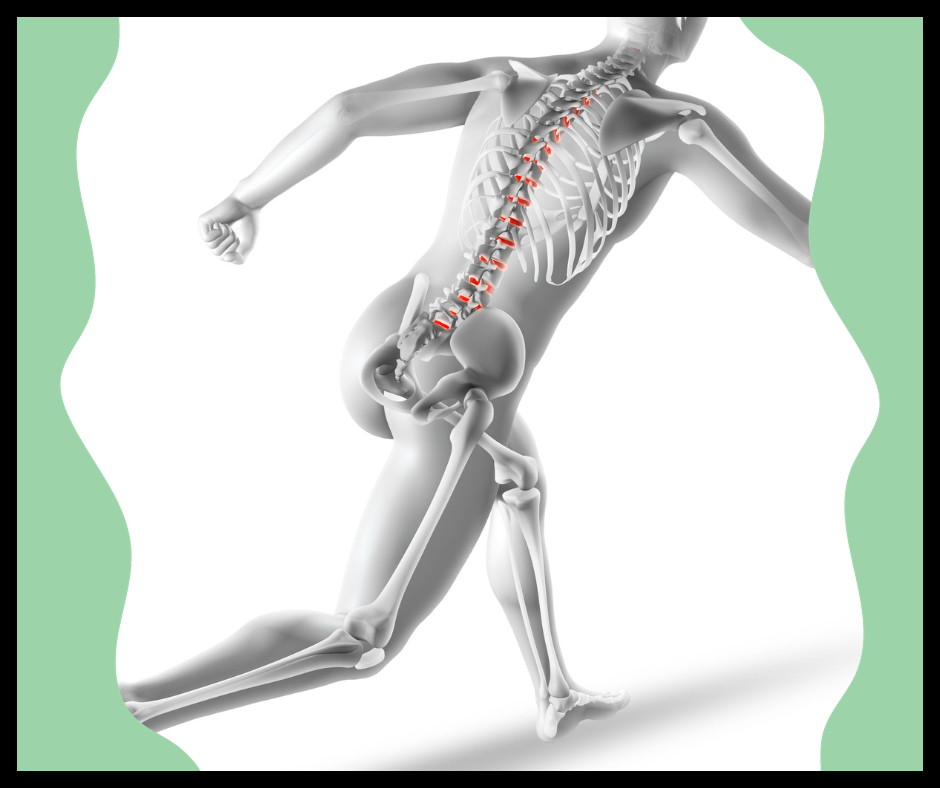
Osteoporosis in elderly people poses a significant health concern, as this condition weakens bones and elevates the risk of fractures, impacting the overall well-being of aging individuals. As bones gradually lose density and strength with age, understanding the specific challenges associated with osteoporosis in the elderly becomes imperative.
Contents
Osteoporosis: life changing
My own mother developed osteoporosis. She worked to improve her bone density, even bowling in several leagues each week. Still, an enthusiastic hug by a long-time friend left her in pain. Her doctor x-rayed and found a fractured rib, thought to be from the hug. Yes, a hug had caused her fragile bone to break. With careful attention and rest, it healed. But we forever remembered to hug gently!
When another family member with osteoporosis fell and broke her hip and leg, the life changing effects of osteoporosis become all too apparent. Years of bone mass loss left her with bones that just crumbled. Her fall amplified this degeneration and left her with tiny pieces of bone that at one time were hip bones. Surgeons removed the bone fragments. But she didn’t have enough leg bone to attach a replacement hip to. Now bedridden, she is learning how to adjust. We hope that she regains enough strength to one day be able to safely move to a wheelchair during the day.
Learn the facts to manage the problem
In this article, we explore the risk factors, causes, diagnostic approaches, and treatment strategies for managing bone fractures and osteoporosis in the aging population, emphasizing the importance of proactive measures to enhance bone health and minimize the potential for fractures.
Video Credits: A.I.M. Fitness-Activities In Motion
Who Is at Risk for Osteoporosis?

Osteoporosis is a condition characterized by the weakening of bones, leading to an increased risk of fractures. While it can affect both men and women, certain individuals are at a higher risk.
Women, especially postmenopausal women, are more prone to develop osteoporosis due to a decrease in estrogen levels, which plays a protective role in bone health. Additionally, individuals with a family history of osteoporosis, a petite body frame, or certain ethnic backgrounds (Caucasian and Asian) may be at an increased risk.
Risk Factors of Osteoporosis in the Elderly
As individuals age, the risk of osteoporosis tends to increase. Aging leads to a gradual loss of bone density and muscle mass, making bones more susceptible to fractures. Other risk factors for osteoporosis that affect the elderly include a sedentary lifestyle, lack of sunlight exposure (resulting in vitamin D deficiency), and chronic conditions such as rheumatoid arthritis or gastrointestinal disorders that may affect nutrient absorption.
What Is the Cause of Osteoporosis?
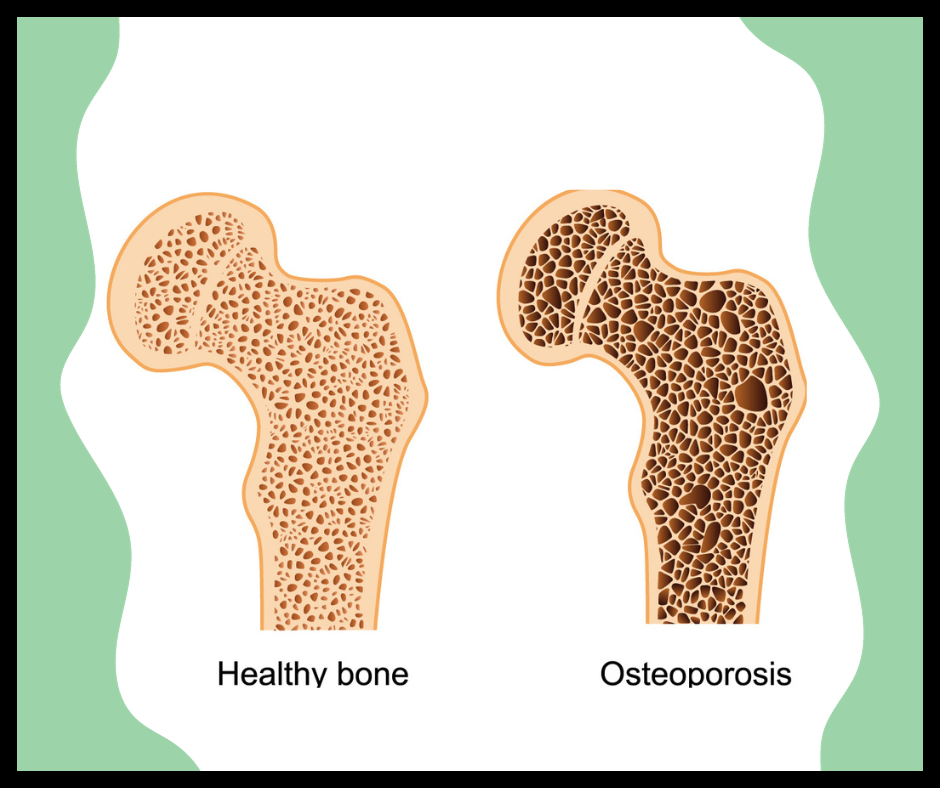
Osteoporosis is primarily caused by an imbalance in the bone remodeling process. Bones are constantly being broken down and rebuilt, and when the creation of new bone tissue doesn’t keep up with the removal of old bone, it results in weakened bones.
Hormonal changes, particularly in postmenopausal women, play a significant role. Other risk factors for osteoporosis include inadequate calcium and vitamin D intake, smoking, excessive alcohol consumption, and certain medications like corticosteroids.
How Is Osteoporosis Diagnosed?
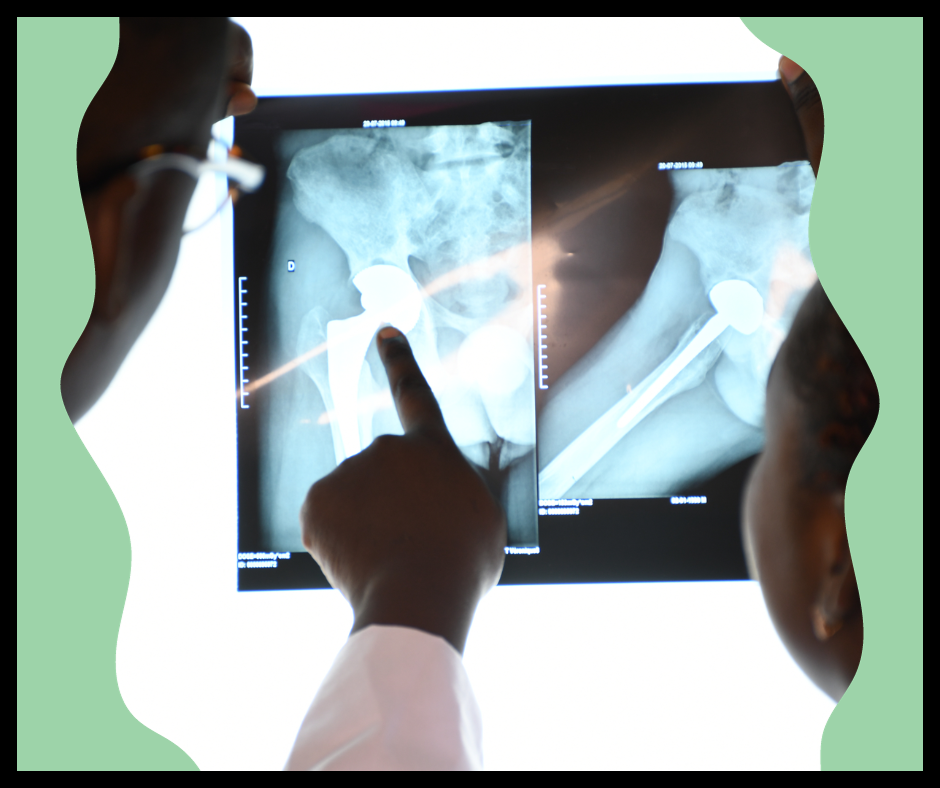
Osteoporosis is often diagnosed through a bone mineral density (BMD) test, typically measured using dual-energy X-ray absorptiometry (DEXA). This non-invasive procedure assesses bone density and helps a bone density test determine the risk of fractures. Medical history, physical examinations, and laboratory tests may also be considered to identify underlying causes of bone loss and contribute to a comprehensive diagnosis.
Causes and Risk Factors

Apart from the aforementioned hormonal changes and lifestyle factors, certain medical conditions (hyperthyroidism, celiac disease) and medications (long-term use of glucocorticoids) can contribute to fracture risk and osteoporosis. Addressing and managing these underlying causes is crucial to prevent further bone loss.
How Is Osteoporosis in Elderly Treated?
The treatment of osteoporosis in the elderly aims to strengthen bones and reduce the risk of fractures. This often involves a combination of medications, such as bisphosphonates or hormone replacement therapy, along with lifestyle modifications. Adequate calcium and vitamin D intake, regular weight-bearing exercises, and avoiding smoking and excessive alcohol consumption are essential components of a comprehensive treatment plan to prevent osteoporosis.
Tips to Prevent Falling
Preventing falls is crucial for individuals with osteoporosis, as fractures resulting from falls can be particularly detrimental. If you want a more detailed guide on Fall Prevention in Elderly, read our article, which provides a complete guide that will surely help you out.
Exercise Regularly

Engage in activities that improve balance, strength, and flexibility. This could include walking, tai chi, or other low-impact exercises. Consult with a healthcare professional before starting any new exercise program.
Maintain Strong Bones
Ensure an adequate calcium and vitamin D intake through diet or supplements if necessary. These nutrients are vital for bone health.
Regular Vision Check-ups

Poor vision can contribute to falls. Have regular eye examinations and update eyeglasses or contact lens prescriptions as needed.
Home Safety Measures
Make modifications to your living space to reduce fall risks. This includes removing tripping hazards such as rugs, keeping pathways clear, and using non-slip mats in bathrooms.
Proper Lighting
Ensure that your home is well-lit, especially in hallways, staircases, and entrances. Consider using nightlights to navigate safely in the dark.
Foot Care
Wear well-fitting, supportive shoes with nonskid soles. Avoid walking in socks or slippers on smooth surfaces.
Medication Management
Review medications with your healthcare provider to identify any that may cause dizziness or drowsiness. Take medications as prescribed and be aware of potential side effects.
Assistive Devices
If necessary, use canes, walkers, or other assistive devices recommended by healthcare professionals to provide added stability.
Stay Hydrated
Dehydration can lead to dizziness and an increased risk of falls. Ensure you are drinking enough water throughout the day.
Be Mindful of Environmental Factors
Be cautious of uneven surfaces, steps, or curbs when walking outside. Watch for wet or slippery conditions and take appropriate precautions.
Regular Health Check-ups
Schedule regular check-ups with your healthcare provider to address any underlying health issues that may contribute to falls.
Balance Training
Consider specific exercises aimed at improving balance, as they can significantly reduce the risk of falling.
The Right Diet to Help in Osteoporosis in Elderly Adults
Diet plays a crucial role in managing arthritis, especially in the elderly. While there is no specific “arthritis diet,” certain dietary factors can contribute to symptom relief and overall joint health. Here are some dietary considerations for addressing arthritis in the elderly:
Anti-Inflammatory Foods

Include foods rich in anti-inflammatory properties to help reduce joint pain and inflammation. These may include fatty fish (like salmon, mackerel, and sardines), walnuts, flaxseeds, chia seeds, and extra virgin olive oil.
Omega-3 Fatty Acids

Incorporate sources of omega-3 fatty acids, which have anti-inflammatory effects. Besides fish, sources include chia seeds, flaxseeds, and walnuts. Consider fish oil supplements, but consult with a healthcare provider first.
Colorful Fruits and Vegetables
Consume a variety of colorful fruits and dark green leafy vegetables rich in antioxidants and vitamins. Berries, cherries, spinach, kale, and broccoli may have anti-inflammatory effects and contribute to joint health.
Calcium and Vitamin D
Ensure an adequate intake of calcium and vitamin D to support bone health. Dairy products, leafy greens, and fortified foods can provide calcium, while sunlight exposure and supplements can help with vitamin D.
Turmeric and Ginger
These spices contain compounds with anti-inflammatory properties. Incorporate turmeric into curries, and use ginger in teas or as a spice in cooking.
Whole Grains
Opt for whole grains over refined carbohydrates. Whole grains like brown rice, quinoa, and whole wheat can provide nutrients that support overall health and may help manage weight.
Protein Sources
Include lean protein sources like fish, poultry, beans, and legumes. Protein is essential for muscle strength, which supports joint stability. If you are vegan, you can get your protein by eating beans, tofu, quinoa, chia, and nuts.
Hydration

Drink plenty of water to maintain joint health. Proper hydration helps keep cartilage lubricated and may contribute to joint comfort.
Limit Processed Foods

Reduce the intake of processed foods, which may contain pro-inflammatory ingredients. Focus on whole, nutrient-dense foods instead.
Moderate Alcohol Consumption
Limit alcohol consumption, as excessive alcohol can contribute to inflammation. For those who choose to drink, moderation is key.
Weight Management

Maintain a healthy weight or lose weight if necessary. Excess weight puts additional strain on joints and broken bones, particularly in weight-bearing areas like the knees and hips.
Limit Sugar and Saturated Fats
Excessive sugar and saturated fats may contribute to inflammation. Limit the consumption of sugary snacks, desserts, and foods high in saturated fats.
Consult a Professional for Severe Cases of Osteoporosis in Elderly Adults

Talking to a doctor about osteoporosis is very important. Osteoporosis is a tricky problem, and doctors know a lot about it. They can do special tests to find out how bad it is and make a plan to help. Doctors are like health detectives who can figure out the best way to make bones strong again.
They also check if there’s a big chance of falling and hurting bones. Doctors help a lot by giving good advice on what foods and exercises are best. So, if someone thinks they have osteoporosis, talking to a doctor is a smart idea to get the best help possible.
Osteoporosis in Elderly Adults is Manageable
I hope you learned that osteoporosis in elderly individuals is manageable with the right type of exercise and diet. It’s important to note that all the remedies mentioned above will only help up to a certain extent.
There are certain instances in which consulting a doctor is essential. Never compromise your health, and I hope everyone stays healthy and happy.
FAQs
What Is Osteoporosis, and Why Is It a Concern for Elderly Adults?
Osteoporosis is when bones become weak, making them more prone to fractures. In elderly adults, the risk of osteoporosis increases due to factors like aging, hormonal changes, and decreased bone density.
What Are the Common Symptoms of Osteoporosis in Elderly Adults?
Osteoporosis often does not show noticeable symptoms until a fracture occurs. However, elderly adults may experience back pain, loss of height over time, and a stooped posture.
How Is Osteoporosis Diagnosed in Elderly Individuals?
Diagnosis involves a bone mineral density (BMD) test, usually conducted through dual-energy X-ray absorptiometry (DEXA). Medical history, physical exams, and sometimes blood tests may also contribute to the diagnosis.
What Are the Risk Factors for Osteoporosis in Elderly Individuals?
Risk factors include aging, postmenopausal status in women, family history of osteoporosis, low body weight, certain medications, and lifestyle factors like lack of exercise and poor nutrition.
Follow our Socials
Connect with your senior parents on Facebook to share memories and updates, and stay in touch with their social circle, fostering a sense of community and support.
Explore the visual appeal of Instagram to document and celebrate your senior parents’ life moments through photos, creating a visually engaging timeline of their experiences for family and friends to enjoy.
Use Pinterest to curate boards filled with helpful tips, activity ideas, and inspiration for enhancing your senior parents’ quality of life, and promoting a vibrant and fulfilling lifestyle.
Stay informed and engaged with your senior parents on Twitter by following relevant accounts, sharing news, and participating in conversations that matter to them, fostering a sense of connection and staying up-to-date on their interests.
Related Readings