Have you ever paused to consider the health of your bones? It’s a topic we often overlook, yet it’s essential. Osteoporosis is a condition that significantly weakens bones. It is surprisingly common and often goes unnoticed until a bone breaks. This guide will explore the often silent yet impactful world of osteoporosis. We’ll uncover why it’s not just a concern for the elderly but a significant health issue for both men and women worldwide. You’ll learn about the intricate details of osteoporosis. These include the factors contributing to it and the effective ways to prevent and manage it. Enjoy reading!
Contents
Understanding Osteoporosis
Causes and Risk Factors of Osteoporosis

Risk Factors
Understanding the risk factors for osteoporosis is critical to prevention. Several factors contribute to this condition:
- Age – Age is a big one. The older you get, the higher your risk.
- Gender – Gender plays a role too. Women are more likely to develop osteoporosis. But men aren’t immune.
- Ethnicity – Ethnicity matters as well. White and Asian women are at a higher risk.
- Body Size – And let’s not forget about body size. Smaller body frames tend to have less bone mass to draw from as they age.
Lifestyle, Diet and Exercise
Lifestyle choices have a significant impact on your bones. Diet is crucial. Not getting enough calcium and vitamin D can lead to weaker bones. Think of these nutrients as the building blocks and reinforcements for your bones. Physical activity is just as important. Weight-bearing exercises help build and maintain bone mass. It’s like a workout for your bones, keeping them strong and resilient. So, a balanced diet rich in calcium and vitamin D and regular exercise can make a big difference in maintaining bone health.
Osteoporosis in Men and Women

Gender Differences
Osteoporosis isn’t just a woman’s issue. It affects men, too, but differently. Women tend to develop osteoporosis earlier, often after menopause. This is due to a rapid decline in estrogen, which is vital for bone health. Men, on the other hand, generally face this risk later in life. Their bone loss starts later and progresses more slowly. However, when men do develop osteoporosis, they often have more severe complications. Both men and women must be aware of their bone health, especially as they age.
Impact of Certain Health Conditions
Certain health conditions can raise the stakes in developing osteoporosis. For women, breast cancer treatments can affect hormone levels, which in turn impacts bone density. Similarly, men undergoing prostate cancer treatments may experience lower testosterone levels. This affects their bones. Rheumatoid arthritis is another condition that can lead to bone loss, affecting both men and women. These conditions don’t just affect your overall health. They directly impact your bones’ strength and durability. I want to discuss these factors with your doctor and take preventive measures to maintain bone health.
The Real Impact of Osteoporosis
Osteoporosis does more than increase the risk of breaking a bone. It leads to serious health complications and affects daily life.
Let’s talkabout what this means for those living with osteoporosis.

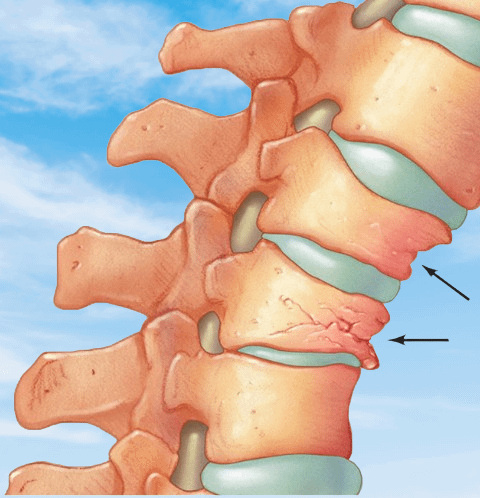
The Threat of Fractures
The most direct consequence of osteoporosis is, of course, broken bones. These aren’t just ordinary fractures. They can be life-altering. Hip fractures are a prime example. They often require surgery and can lead to long-term disability. Spine fractures are another primary concern. They can lead to severe back pain and a decreased quality of life. Even a simple wrist fracture can impact your ability to perform daily tasks. These fractures can happen from minor falls, sometimes even from everyday activities.
Beyond the Breaks
But it’s not just about the fractures. Osteoporosis can lead to changes in posture. Think of a stooped or hunched back. This isn’t just an aesthetic issue. It can cause chronic pain and reduce mobility. The psychological impact is also significant. Fear of falling can lead to decreased activity, weakening the bones and creating a vicious cycle. For many, osteoporosis leads to a loss of independence, which can be devastating. Osteoporosis isn’t just a bone issue. It’s a severe condition that can affect every aspect of life. But there’s hope. With the proper management and lifestyle changes, its impact can be minimized.
Osteoporosis Diagnosis and Testing
Detecting osteoporosis early is vital for effective management. Discuss how doctors diagnose this silent disease and why timely testing is crucial.

The Role of Bone Density Tests
The most common way to diagnose osteoporosis is through a bone density test. It’s a simple, non-invasive procedure that measures how much bone you have. This test is crucial for those with risk factors for osteoporosis. It helps doctors assess your bone health and predict your risk for future fractures. Think of it as a snapshot of your bone strength. The results can show whether you have average bone density, low bone mass (osteopenia), or osteoporosis.
Identifying Early Signs
Why wait for a broken bone to learn about your bone health? Early stages of bone loss can be silent. This is where regular check-ups come in. They can help catch signs of weakening bones before a fracture happens. This is especially important for postmenopausal women, older adults, and those with a family history of osteoporosis. The earlier you know, the sooner you can strengthen your bones.
When to Get Tested
So, when should you consider a bone density test? It’s typically recommended for women over 65 and men over 70. But if you have risk factors like a family history of osteoporosis, early menopause, or certain medical conditions, your doctor might suggest testing earlier. Also, getting tried is a good idea if you’ve experienced a bone fracture after a minor injury.
Prevention and Management of Osteoporosis
Preventing and managing osteoporosis isn’t just possible; it’s essential. Here are some practical ways to keep your bones strong and reduce the risk of fractures.

Building and Maintaining Strong Bones
Building strong bones, especially before age 30, is the key to preventing osteoporosis. After that, it’s about maintaining bone strength. Calcium and vitamin D are your bones’ best friends. They’re crucial for bone health. Think of calcium as the building block and vitamin D as the helper that lets your body absorb calcium. Dairy products, leafy greens, and fortified foods are great calcium sources. For vitamin D, sunlight is your ally, along with fatty fish and fortified foods.
The Power of Exercise
Exercise isn’t just for muscles. It’s vital for bones, too. Weight-bearing activities, like walking, jogging, and strength training, help build and maintain bone density. They’re like a workout for your bones, keeping them strong and resilient. Aim for at least 30 minutes of exercise most days of the week. It’s not just good for your bones but for your overall health, too.
Lifestyle Choices Matter
Smoking and excessive alcohol consumption can harm your bones. Quitting smoking and limiting alcohol can significantly improve your bone health. It’s also about maintaining a healthy weight. Being underweight can increase the risk of bone loss and fractures. A balanced diet and regular exercise can help you maintain a healthy weight and strengthen your bones.
Treatment Options for Osteoporosis
When it comes to treating osteoporosis, there’s no one-size-fits-all solution. But with the right approach, you can manage this condition effectively.

Medications
Several medications can help slow bone loss and increase bone density. These include bisphosphonates, typically the first choice for treating osteoporosis. They work by slowing down the process that breaks down bone tissue. For postmenopausal women, hormone-related therapy might be an option. It can help maintain bone density. Remember, each medication comes with its own set of benefits and risks. I think it’s important to talk about these with your healthcare provider to find what works best for you.
Physical Therapy and Lifestyle Changes
Physical therapy can be a game changer in treating osteoporosis. It helps improve balance and strength, reducing the risk of falls and fractures. Incorporating specific exercises tailored to your needs can make a big difference. Alongside medication and therapy, lifestyle changes play a vital role. This includes maintaining a diet rich in calcium and vitamin D, and regular weight-bearing exercises. Also, avoiding smoking and excessive alcohol consumption is beneficial.
The Role of Supplements
Sometimes, getting enough calcium and vitamin D through diet alone is challenging. That’s where supplements come in. They can help fill the gap. However, talking to your doctor before starting any supplements is very important. They can help determine the correct dosage and ensure it doesn’t interfere with other medications.
Credit: @Amgen
Embracing Life with Osteoporosis
Living with osteoporosis doesn’t have to limit your life. You can still enjoy a whole, active lifestyle with the right approach.
First, staying informed is crucial. Understanding your condition helps you make more intelligent choices. I would like to let you know that regular check-ups and communication with your doctor are essential. They keep you on track with your treatment and prevention strategies.
Adapting your home to prevent falls is essential, too. Simple changes can make a big difference. Consider securing rugs, improving lighting, and installing grab bars in the bathroom. These adjustments can help prevent falls, a major cause of fractures in people with osteoporosis.
Nutrition plays a significant role in managing osteoporosis. A diet rich in calcium and vitamin D is essential for bone health. Leafy greens, dairy, and fortified foods are great options.
And let’s remember about exercise. Weight-bearing and muscle-strengthening exercises help maintain bone density and strength.
It’s also about staying connected and active. Engaging in social activities and hobbies keeps your mind and body sharp. Plus, it boosts your mood and overall well-being.
Remember, having osteoporosis doesn’t mean giving up the things you love.

Wrapping It Up
Now, let’s reflect on what we’ve learned.
Osteoporosis is more than just a condition. It’s a call to pay attention to our bone health. Whether through prevention, management, or treatment, we can do much to combat this silent disease.
Remember, knowledge is your greatest ally. Adopting a healthy lifestyle rich in calcium and vitamin D and regular exercise is crucial.
And if you’re living with osteoporosis, know that with the right approach, you can still lead a vibrant and fulfilling life.
I would say that regular check-ups and open conversations with your healthcare provider are essential. They help you stay on top of your bone health and make informed decisions.
Whether looking to prevent or manage osteoporosis, the journey is about making choices supporting your bones. So, let’s not take our bone health for granted.
We can face osteoporosis head-on by staying informed, proactive, and positive. It’s about taking control of our health, one step at a time, for a stronger, healthier future.
Thank you for sticking with us on this article. Here’s to strong bones and a healthier you!
Frequently Asked Questions
What Are the Main Causes of Osteoporosis?
Osteoporosis is often due to age-related changes, hormonal imbalances, and genetic factors. Reduced estrogen in postmenopausal women and lower testosterone in men are vital contributors. A family history of osteoporosis, certain medical conditions like rheumatoid arthritis, and lifestyle choices like low calcium intake and lack of exercise also play significant roles.
Can Osteoporosis Be Prevented?
Yes, there are effective ways to reduce the risk of developing osteoporosis. Maintaining a diet rich in calcium and vitamin D is crucial. Regular weight-bearing exercises strengthen bones. Avoiding smoking and excessive alcohol use also helps. For those at higher risk, like postmenopausal women, preventive medications might be recommended.
How Is Osteoporosis Diagnosed?
Osteoporosis is commonly diagnosed through a bone density test. This test measures the amount of bone mineral density and helps identify early stages of bone loss. It’s recommended for women over 65, men over 70, and those with risk factors for osteoporosis at a younger age. Early diagnosis is critical for effective management of the condition.
Learn More About Senior Care!
Learn about the best types of walkers for elderly parents and much more with us. We provide essential tips and tricks for caring for your senior loved ones. Follow us on social media for practical advice and supportive information.
Facebook: https://www.facebook.com/sr.parents
Instagram: https://www.instagram.com/seniorparents/
Twitter: https://twitter.com/senior_parents
For more on senior care, visit our site: SRParents.com. Empower yourself with the knowledge to provide the best care for your elderly parents!
Read More