Type 2 diabetes and osteoporosis are becoming more common, affecting more lives globally. This rise is mainly due to factors like sedentary lifestyles, bad diets, and an increase in the aging population. With more people facing these issues, it is vital to grasp how they affect the human body.
While Type 2 diabetes messes with blood sugar, osteoporosis weakens our bone health. However, it doesn’t stop there. In addition to disrupting blood sugar levels, diabetes also messes with our bone density, creating a dual health problem.

This article aims to shed light on Type 2 diabetes and osteoporosis. We will explain how they sneak into our lives, their impact on our bodies, and how to prevent them.
By the end, you will have a clearer picture of how to keep these health concerns at bay. So, get ready to tackle the rising challenges of Type 2 diabetes and osteoporosis!
Contents
Understanding Type 2 Diabetes Mellitus
Type 2 diabetes is the most common form of diabetes. It is a chronic condition caused by excessively high blood glucose levels. This glucose, derived from our food, is the primary energy source. Insulin also aids in the entry of glucose into cells for energy use.
However, in type 2 diabetes, our body either doesn’t make enough insulin or is unable to use it well. Consequently, glucose keeps building up in the bloodstream, leaving cells with inadequate amounts.
Who Is At A Higher Risk of Getting Type 2 Diabetes?
Type 2 diabetes can affect anyone, no matter their age. However, the condition tends to increase in middle-aged and older adults. People in their 40s or older are more at risk, especially if they have a family history of diabetes or are carrying extra weight.
Type 2 diabetes is more common in certain ethnic groups like African Americans, American Indians, and Pacific Islanders.
Moreover, lack of physical activity and specific health issues can also increase the risk of type 2 diabetes. For example, if you have had prediabetes or gestational diabetes during pregnancy, that can make you more prone to it, too.
Symptoms of Type 2 Diabetes Mellitus
The symptoms of type 2 diabetes emerge gradually. You can be living with T2D for years without realizing it. However, When symptoms become noticeable, they often include:
- Increased Thirst: Individuals with T2D may experience more thirst. They feel the need to drink more water than usual.
- Frequent Urination: T2D often increases the need to urinate, disrupting daily activities.
- Feeling More Hungry: people with T2D may feel hungrier than usual, even right after eating.
- Unintended Weight Loss: Even though you might feel hungrier, some people with T2D may lose weight without meaning to.
- Fatigue: You might feel tired and need more energy, making it hard to do your daily activities.
- Blurred Vision: Blurred or distorted vision can occur, affecting the clarity of eyesight.
- Slow-Healing Sores: Wounds or sores may take longer to heal than expected.
- Frequent Infections: Individuals with type 2 diabetes may be more susceptible to infections.
- Numbness or Tingling: Some may feel a tingling or numbness, especially in their hands or feet.
- Areas of Darkened Skin: Dark patches on the skin, especially in the armpits and neck, could appear.
It is crucial to be aware of these signs and symptoms. Remember that catching T2D early and taking care of it is vital for your overall health. This helps prevent complications linked to T2D. If you see these symptoms, talk to a doctor for a proper check-up and diagnosis.
Understanding Osteoporosis
Osteoporosis is a condition that affects our bone health. It occurs when there is a decline in bone mineral density, bone mass, or changes in bone structure and strength. This weakening can raise the chances of bone fractures.
Osteoporosis, known as a “silent” disease, usually does not show symptoms. You might not realize you have it until you experience a bone break. It stands out as the primary reason for fractures in postmenopausal women and older men, with fractures occurring in any bone but commonly affecting the hip, vertebrae in the spine, or wrist.
Who Gets Osteoporosis?

Osteoporosis can affect people of any race or ethnic background, both women and men. It might happen at any age, but the chances of getting it increase as you age. In many women, it starts developing a year or two before they go through menopause.
Non-Hispanic white and Asian women are more likely to get osteoporosis. African American and Hispanic women have a low risk but are still at significant risk. Among men, it’s more common in non-Hispanic white men.
Certain medicines, like some cancer drugs and steroids, may make the risk of osteoporosis higher. Since osteoporosis often affects women more than men, many men think they are safe. However, both aging men and women can have osteoporosis, regardless of their backgrounds.
Sometimes, kids and teens get a rare type called idiopathic juvenile osteoporosis. Doctors don’t know why it happens, but most kids get better without treatment.
Symptoms of Osteoporosis
As mentioned earlier, osteoporosis is a silent disease. It usually has no noticeable symptoms during the initial stages of bone loss. However, as it weakens the bones, signs and symptoms may become evident, including:
- Back Pain: This can result from a broken or collapsed bone in the spine. Individuals may experience persistent back pain.
- Loss of Height Over Time: Osteoporosis can lead to a gradual loss of height as the bones in the spine weaken and compress.
- Stooped Posture: Weakening of the bones may cause a stooped or hunched posture. It alters the natural alignment of the spine.
- Increased Fracture Risk: Osteoporosis makes bones more delicate, making them fracture easily. Even a little bump or pressure on the bones might cause fractures for some people.
Awareness of these signs is essential, especially as osteoporosis progresses. Early detection and management are crucial.
It may help prevent further bone loss and reduce fracture risk. If you see any of these signs, consult your doctor for a thorough evaluation and appropriate diagnosis.
Video Credit: Osteoporosis Canada
Does Diabetes Cause Osteoporosis?
Diabetes is not the cause of osteoporosis. However, having diabetes mellitus, especially diabetes 1, increases your risk of developing osteoporosis.
Individuals with diabetes mellitus generally have weaker and poorer bone density. It makes them more prone to bone fractures.
Factors that raise the risk of a bone fracture include:
- The length of time you have had diabetes.
- Blood sugar level management, especially for individuals with low blood sugar.
- Whether you use insulin or not, that can tie in with low blood sugar, leading to higher risk.
The Link Between Type 2 Diabetes and Osteoporosis
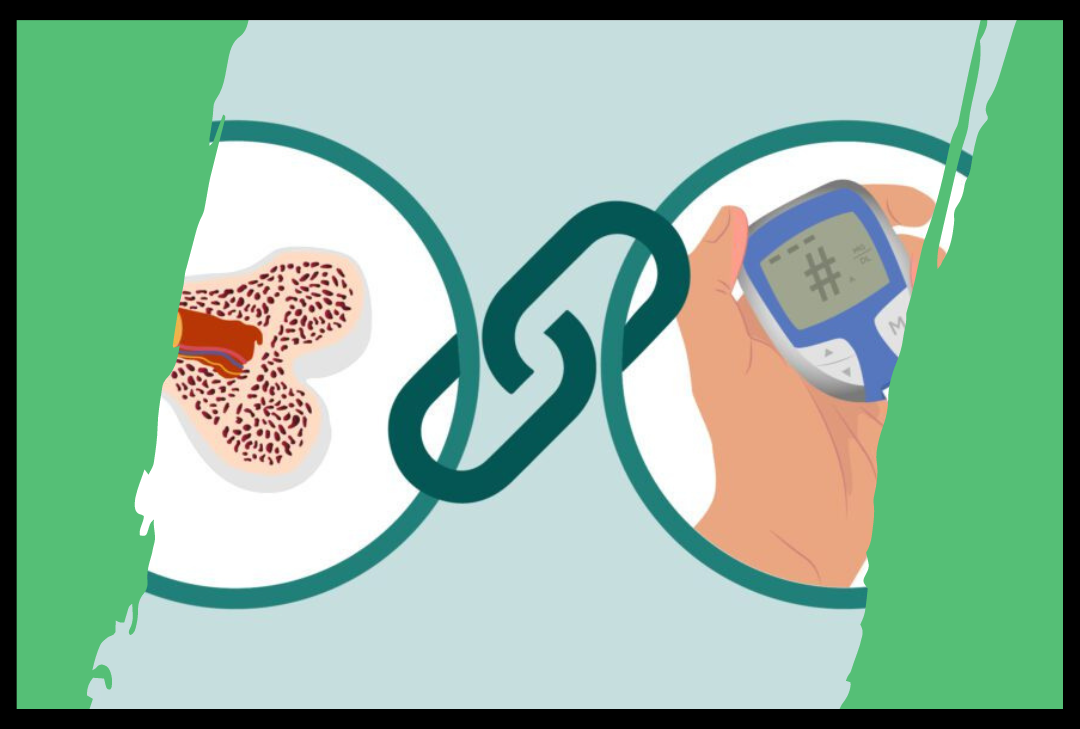
Type 2 diabetes and osteoporosis have something in common. Besides well-known health issues, type 2 diabetes also affects bone metabolism and bone quality.
Diabetes increases osteoclast function (cells that break down bones) but decreases osteoblast function (cells that build bones). This imbalance causes bones to lose strength faster, leading to osteopenia and osteoporosis (a condition where the bones become weaker and prone to fractures).
While it may seem surprising, research suggests that diabetic patients have an increased risk of osteoporosis. Here’s how the connection works:
Type 2 Diabetes and Bone Density
Patients with type 2 diabetes often have a higher bone mineral density. However, studies suggest that they have a higher risk of developing a bone fracture.
Type 2 diabetes and bone density are interconnected. Having Type 2 diabetes mellitus doesn’t just affect your blood sugar but also your bones. In T2D, the hallmark is insulin resistance, in which the body’s cells don’t respond to insulin. Insulin regulates blood sugar levels and is essential for bone health.
There’s a two-sided impact on the bones in Type 2 diabetes. The spongy part of bones, called trabecular bone, tends to weaken (low bone mass), while the outer layer, cortical bone, gets stronger (increased bone mass).
Why does this happen? Well, blame it on osteoblasts’ decreased number and function, the cells that build bones. With less work from these cells, making new bone becomes a struggle, especially for the spongy part.
Moreover, patients with Type 2 diabetes often have lower levels of vitamin D. This vitamin is crucial for supplying calcium and phosphate, essential for bone health. However, reduced vitamin D levels disrupt the balance of these minerals in your bones, increasing the risk of fractures.
Chronic Inflammation
Both Type 2 diabetes and osteoporosis share a common thread of chronic inflammation. This ongoing inflammation impacts our bone health. Chronic inflammation influences the delicate equilibrium between bone formation and resorption. The condition of diabetes may contribute to expedite bone loss and an increased osteoporosis risk.
Medications
Some drugs that help with Type 2 diabetes, like glucocorticoids, can affect bone density. Glucocorticoids are often given to manage inflammation linked to diabetes.
However, these medics can interfere with the normal bone remodeling process. As a result, it leads to decreased bone density and an elevated risk of osteoporosis.
Weight
Healthy weight is crucial for bone mass and density. Being underweight or having a small body frame can negatively impact bone density, increasing the risk of osteoporosis. In contrast, adequate weight supports bone strength and resilience.
Smoking
Smoking poses a significant risk for osteoporosis and bone fractures. The harmful substances in tobacco can interfere with bone cells and reduce bone mass. It increases the risk of bone fractures.
Alcohol
Excessive alcohol consumption is linked to impaired calcium and vitamin D absorption. Remember that both these minerals are essential for bone mineral density and development. However, alcohol disrupts our body’s ability to absorb these vital nutrients, raising the risk of osteoporosis when coupled with diabetes.
Beyond specific mechanisms, Type 2 diabetes mellitus and osteoporosis often coexist. Both conditions have a few shared risk factors.
For example, aging is a significant factor for both conditions. As individuals age, they may be more prone to the dual impact of diabetes and osteoporosis.
Moreover, a sedentary life is pretty standard in both Type 2 diabetes and osteoporosis. It can impact bone formation and increase the risk of diabetes.
Additionally, poor nutrition is another shared risk factor. Poor dietary choices can make dealing with these health issues even tougher.
How to Manage Your Bone Heath if You Have Diabetes?
Good news! The tips for managing diabetes and blood sugar are pretty much the same as those for taking care of osteoporosis. So, let’s start with these helpful strategies.
Embrace a Healthy, Nutritious Diet
A nutritious diet is critical for managing type 2 diabetes and osteoporosis. Studies suggest that poor dietary habits can increase the risk of osteoporosis.
However, following healthier eating habits may help decrease the risk. In particular, vitamin D deficiency in many people with diabetes stresses the need for a well-rounded diet.
Thus, it is vital to embrace a healthy diet. Aim for a balanced diet with many fruits, veggies, fish, whole grains, and legumes. While more research is needed to grasp how diet affects bone metabolism in diabetic people, many people with diabetes may lack vitamin D.
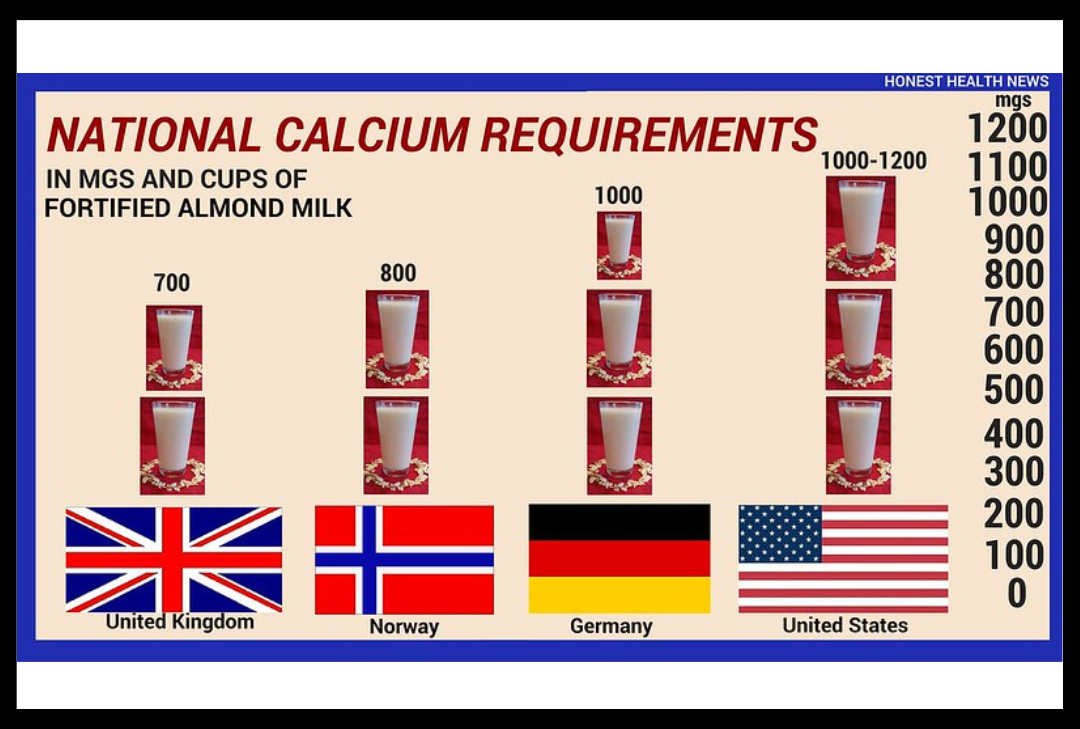
Calcium and vitamin D are critical for strong bones. So ensure that you are getting enough of these nutrients from your diet.
Moreover, for women under 50 and men under 70, the target calcium intake is 1,000 mg per day. It should be increased to 1,200 mg daily for women over 51 and men over 71. In contrast, the recommended vitamin D intake is 400-800 IU daily for adults under 50 and 800-1,000 IU daily for those aged 50 and above.
Exercise Regularly and Maintain a Healthy Weight
Regular exercise is vital for managing weight in diabetes mellitus. Patients with Type 2 diabetes should emphasize activities that promote muscle gain. It also helps them to combat bone fragility and any decreases in bone mass that may come with weight loss.
Moreover, regular exercise is also crucial for preventing osteoporosis. Not only does it promote bone formation in patients with diabetes, but it also prevents falls. To address diabetes and safeguard bone quality, plan a diverse workout routine.
To address diabetes and safeguard bone quality, plan a diverse workout routine. Studies show that resistance exercises, in particular, can help preserve both bone and muscle mass. Combining resistance exercises with weight-bearing aerobic activities may also be beneficial in preventing excessive bone loss.
Quit Smoking to Prevent the Risk of Osteoporosis
Smoking can weaken bones and heighten the risk of fractures. Research indicates that smoking is linked to an increased risk of osteoporosis in individuals with type 2 diabetes. Additionally, many smokers engage in other unhealthy habits that impact both diabetes and bone health, such as reduced physical activity and poor diet choices.
If you smoke, it’s strongly recommended to quit. A study suggests that quitting smoking may help regain bone mass that was previously lost due to smoking.
Consult your doctor for assistance with quitting. They can provide guidance and discuss the potential use of smoking cessation aids to support you in your journey to quit smoking.
Quit Smoking to Prevent the Risk of Osteoporosis
Smoking can weaken bones and heighten bone fracture risk. Research indicates that smoking is linked to an increased risk of osteoporosis in those with Type 2 diabetes.
In addition, many smokers engage in other unhealthy habits that can trigger diabetes and decreased bone mass. These may include reduced physical activity and poor diet habits.
If you are a smoker and have diabetes mellitus, it is strongly recommended to quit smoking. Some studies show that quitting smoking may help regain bone mass that was lost due to smoking.
Keep Your Alcohol Consumption in Check
Alcohol intake is another culprit that may cause osteoporosis. Studies show that chronic and excessive alcohol consumption raises the risk of osteoporosis. Heavy drinking is linked with low bone mineral density and weakened bones.
Moreover, excessive alcohol use also impacts your other lifestyle habits. Alcohol consumption influences your eating habits, causing adverse impacts on bone quality.
However, if you choose to drink, do so in moderation. It should be just one drink daily for women and two for men.
Moderate alcohol intake might have potential benefits, including improved blood sugar and insulin sensitivity. However, it doesn’t mean you should start drinking if you currently do not.
Wrapping Up: Type 2 Diabetes and Osteoporosis
To sum up, having both type 2 diabetes and osteoporosis means looking at health in a detailed way. Even if the signs are not clear, finding problems early is essential. Taking care of each condition’s unique symptoms is crucial for overall health.
The coexistence of T2D and osteoporosis needs a holistic approach to health. Timely medical attention and lifestyle adjustments can significantly impact overall well-being.
In managing bone health with diabetes, adopting a nutrient-rich diet and incorporating regular exercise emerge as pivotal strategies. These aid in blood sugar control and contribute to maintaining robust bones.
The journey towards optimal health involves a proactive and informed approach. By understanding the nuances of T2D and osteoporosis, individuals can make empowered choices, fostering a life marked by vitality and resilience.
FAQs
What is the average bone mineral density level in adults?
The average bone mineral density level in adults is usually defined as a T-score. A T-score between +1 and -1 means your bone mineral density level is normal and healthy. However, if the T-score falls between -1 and -2.5, it indicates a low bone density.
Similarly, if it goes below -2.5, it suggests osteoporosis. Remember that what’s considered normal for bone density might depend on how the test is done and the group of people being looked at. Individual results should be discussed with a healthcare professional for a comprehensive understanding.
What are the types of vertebral fractures?
Vertebral fractures have four main types. The first is compression fracture.
It occurs when the front part of a vertebra collapses, leading to a compressed appearance. The second type is a wedge fracture, where one side of the vertebra loses height, creating a wedge-shaped impression.
Another type is a burst fracture, where the vertebra breaks in different directions, causing fragments to spread. Lastly, there is the crush fracture, where the entire vertebra is compressed, leading it to lose its standard shape. Vertebral fractures can happen due to various factors, including osteoporosis and trauma.
How does low bone mass increase the risk of fractures?
Low bone mass raises the risk of fractures, increasing bone fragility and weakening them. When bone density is low, even a minor impact or stress on the bones can lead to fractures. When you have low bone mass, your bones become weaker and more likely to break.
What are common metabolic bone diseases?
Common metabolic bone diseases include osteoporosis, osteomalacia, and Paget’s disease. These can affect the bones, leading to problems like fractures, weakness, and pain.
Welcome to Senior Parents – Your
Trusted Companion in Elderly Health!
We are your go-to place for practical tips and insights on elderly health. Our platform addresses common health issues that seniors may face. We offer helpful tips and tricks so you can enhance the well-being of your loved ones.
Explore our informative articles that cover a wide range of topics, from managing chronic conditions to promoting mental and physical health in older people.
At Senior Parents, we believe in the power of knowledge and community. Our goal is to help you with the information needed to navigate senior health challenges. Whether you are a caregiver or a senior, we are here to guide you through aging with expert advice.
Join us to stay updated on the latest articles. Engage with fellow readers and receive exclusive tips for senior care. Let’s work together to ensure the best possible health and happiness for our beloved seniors.
Facebook: www.facebook.com/sr.parents
Insta: www.instagram.com/seniorparents
Pinterest: www.pinterest.com/seniorparents
Twitter: twitter.com/senior_parents